The CAQH Index addresses how reducing the burdens of administrative costs could reduce healthcare spending.
The 49-page CAQH Index Report is incredibly insightful and full of information, but in order to make it more digestible, we’ve pulled some statistics we found most valuable. All of the data in this post is directly from the report and the full report is available on their website.
The Current State of Administrative Costs
The healthcare industry spends an estimated $350 billion annually on administrative costs – due to its complexity. Of these costs, $40.6 billion is associated with transactions that are tracked by the CAQH Index. The Index states that $13.3 billion or 33% of those tracked costs could be saved by completing the transition from manual and partially electronic processing to fully electronic processing.
The Administrative Process
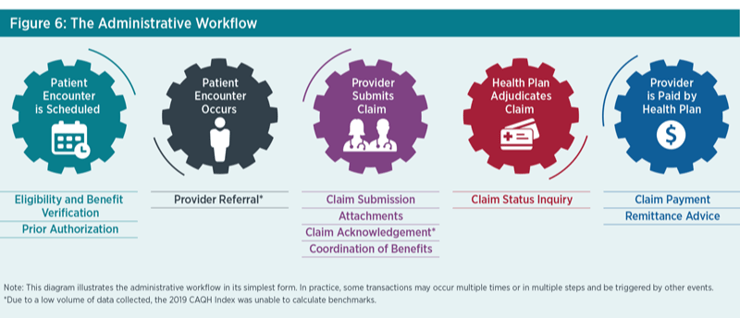
*The Administrative Workflow Figure 1. Source: 2019 CAQH Index
The medical industry could save as much as $42.45 (including $29.27 for providers and $13.18 for plans) for a single patient encounter by requiring all eight of the transactions tracked to use a fully electronic workflow.
The greatest per transaction savings from moving from manual to fully automated can be realized in the following areas:
- Prior authorization ($12.31)
- Claim status inquiry ($7.72)
- Eligibility and benefit verification ($7.55)
Eligibility and Benefit Verification
Eligibility and Benefit Verification transactions represent the highest annual spending and savings opportunity. This is due to the large overall volume of this transaction and the volume conducted through partially electronic web portals. This transaction accounts for 47% of the total medical industry spend. Providers have indicated that complicated benefits have resulted in additional points of contact with plans, and providers check on eligibility and benefit information multiple times throughout an encounter.
The medical industry could save 85 cents per transaction by conducting eligibility and benefit verification electronically using the HIPAA standard as opposed to a web portal. In addition, medical providers could save 8 minutes per transaction by switching to fully electronic processing – adding even more savings.
Prior Authorization
Prior Authorization is the costliest and most time consuming to conduct manually. Industry adoption of electronic prior authorization is lower than other transactions due to provider awareness, vendor support, inconsistent use of data content allowed in the standard, state laws mandating manual processes, and lack of an attachment standard to support the exchange of medical documentation.
Moving from web portals to fully electronic could save $2.11 and 17 minutes per transaction, as the time is slashed from 21 minutes to four.
Claim Submission
Claim submission continues to have the highest electronic adoption rate, which is critical to sustain in order to control costs. The rate of fully electronic processes has remained steady at 96% compared to the prior report. Even though this transaction is mostly automated, there is still $635 million in savings opportunity through complete automation.
Electronic Attachments
Serving as a bridge between clinical and administrative data, attachments are critical to the success of value-based payment models. As we transition from fee-for-service to value-based payment, there is a clear need for clinical and administrative systems to streamline the exchange of information to support patients, providers and plans.
Although attachments are primarily exchanged through costly and time consuming manual methods, the volume of these transactions is low, accounting for less than one percent of the total volume of administrative transactions. An average of $4.50 and 11 minutes of staff time is spent on each manually processed attachment.
Coordination of Benefits
Adoption of electronic coordination of benefits has the second highest adoption rate and the fastest growth among the transactions. The spend associated with this transaction is the lowest among the medical industry administrative transactions reported. Medical plans could save an additional $16 million by switching their remaining manual COB transactions to electronic.
Claim Status Inquiry
Claim status volume decreased for the second year in a row. This is partially because providers now only check on the status of a claim after a minimum of 30 days versus more frequently, which may be due to quicker adjudications and payments from plans.
This transaction accounts for 15% of medical spend and is the second most expensive transaction to conduct manually ($10.13) and electronically ($2.41). On average, it takes 12 minutes to conduct a manual claim status inquiry and only four minutes for electronic.
Claim Payment
The volume of claim payments rose 18%, however, claim submission volume is higher because payments are often made in bulk where one payment is associated with multiple claims.
Paper checks, on average, take five minutes to process compared to three minutes electronically. By conducting claim payments electronically, the medical industry could save $135 million annually.
Remittance Advice
The adoption of electronic remittance advice (ERA) transactions increased slightly from the last report. Roughly 20% of the total spent on administrative transactions is around remittance advice.
On average, medical providers reported that an ERA required two minutes of staff time compared to seven minutes when conducting the transaction manually.
The Industry Call to Action
To support adoption of fully electronic transactions that can accommodate evolving market needs, limit cost and reduce burden, CAQH proposes the following actions for the industry to help maintain and improve upon the achievements accomplished to date:
- Focus efforts to reduce provider burden.
- Accelerate standards and operating rule development to support the harmonization of administrative clinical data exchange.
- Need for vendor adoption of all standards and operating rules.
- Expand research related to the administrative workflow.
Quadax can help your organization automate any of these transactions, whether you’re a hospital, laboratory or physician practice. Let's talk!


