Make the patient experience part of your strategy and provide patients with the pricing transparency they want.
By definition, consumerism is a social and economic order that encourages the acquisition of goods and services in ever-increasing amounts. In an abstract sense, it is the consideration that the free choice of consumers should strongly direct the choice of what is available and how, which then directs the economic organization of a society.1
In our world of healthcare and independent clinical labs, consumerism (relative to our business purposes) is the equivalent of, or can be defined as, patients demanding price transparency on their lab testing. This demand in transparency is a result of more and more people in the U.S. having to spend more out-of-pocket on their healthcare due to a variety of factors. Why?
LEADING CAUSES OF CONSUMERISM IN HEALTHCARE
With healthcare spending on the rise, employers are tasked with trying to control costs, which is often passed on to the insured with an increase in premiums and deductibles. A Dark Daily white paper stated that annual premiums for individual coverage increased by 3%.2 In an effort to keep premiums low but keeping the cost burden off the insurance company, we have seen a steady increase in deductibles. And a Quadax white paper stated, “back in 2009, the average deductible was $533 for a single person, but has since risen by over 150% to $1,350 in 2018.”3
The same Dark Daily white paper also reported that the uninsured rate among working-age adults in the U.S. increased to 15.5% in 2019. And, among the 19 states that have not expanded their Medicaid programs, 21.9% of residents remain uninsured. In essence, increasing premiums and deductibles along with the un-or under insured have given rise to an overall increasing level of patient responsibility.
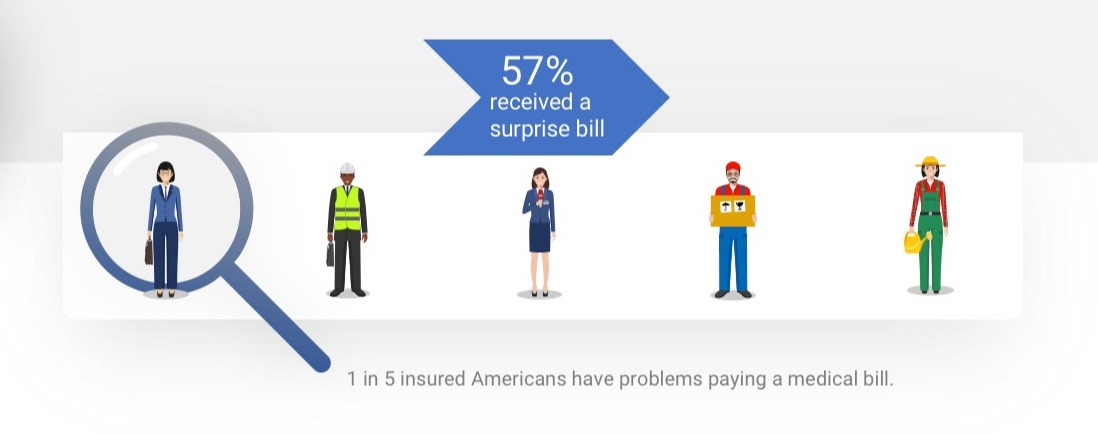
We know that denied claims, if not submitted or worked properly, can lead to a surprise bill back to the patient they may or may not be prepared for. According to a survey out of the University of Chicago, a recent poll reported 57% of American adults have been surprised by a medical bill that they thought would have been covered by insurance.4 And according to a credit organization, statistics show 1 in 5 insured Americans have problems paying their medical bills, often because they are not clear on the cost and are not financially prepared, which can lead to debt or problems paying other bills.5
As such, CMS is now legislating to protect patients from surprise billing – the financial result of a patient receiving in-network care by an out-of-network provider (including ER provider, anesthesiologist, radiologist, and pathologist), often the bill being the difference between the charged and the allowed amount of a service. Patients are demanding more price transparency, so hospitals and some labs are now required to post what they charge for services on their website in response to this legislation.
REAL WORLD PROVIDER CHALLENGES
While there is a desire to provide some level of pricing transparency to patients, it is not without challenges, especially when working with health systems or the providers tied to them. For example, there may be no visibility to your pricing within the systems they use – EMR, practice management solution or other order-entry system. Automation and integration with their systems would alleviate this, but this is extremely expensive and requires IT resources. Thus, your next best option is either through yet another physician portal or via a paper req – both with their own set of challenges, such as inducing more “portal fatigue” or dealing with incomplete reqs. Therefore, you may be relying on your sales team to communicate pricing and financial assistance packages, which also comes with its own set of challenges and may not be the best path forward. Labs want to maintain compliance with their contracted payers for reimbursement and yet at the same time have to hold patients accountable for their co-insurance. Somehow you have to strike a balance between compliance and price transparency.
In order to meet the demand for price transparency, remain compliant with payers, and adhere to current or expected government mandates, many hospitals and labs are investing in tools to help uncover patient financial responsibility in advance, helping them to remain competitive as well as support revenue growth.
HOW LABS CAN MOVE FORWARD
The key take away is that you don’t want someone else driving this movement of consumerism, which is what hospitals and ambulatory centers are experiencing. Labs have not yet been hit with regulations and they may not. But the demand for pricing transparency is coming if you are not already experiencing it. Needless to say, consumerism is a driving factor in healthcare today and labs will see their share. In order to stay competitive, you need to get ahead of it. The good news is you can!
At the end of the day, the movement towards increased pricing transparency means that labs need to evolve and include/re-think the patient experience into their strategy. However, labs don’t often interact with the patient. Instead, labs typically interact with the physician’s office and the insurance company, managing the noise of verifying insurance coverage and eligibility, obtaining prior authorization, and proving medical necessity. Simultaneously, labs may be waiting to run a test or release results of a test while this information is being gathered and completing the patient financial clearance process.
Labs also have to consider the communication between the provider and the patient, which in the world of lab testing, is reliant on how the lab manages the provider’s expectations.
Most importantly, this new trend tells us patients want a say in their care when finances are involved. They want to know their financial responsibility in advance, where possible. Often times, it will be up to the provider to deliver this information, but labs will need to do their due diligence to provide those details. Not only will it provide price transparency, but it can also impact treatment decisions and care. For example, if a patient’s out-of-pocket or financial responsibility is $1,500 and they have not met their deductible, this positions the lab to lead what can be a difficult conversation with the patient on next steps and simultaneously consider the sensitivity of the provider on providing diagnostic information. Consequently, the need for a methodology used to obtain out-of-pocket information can also give the lab peace of mind on the likelihood of the patient paying their lab bill.
In order to make the patient experience part of your strategy, you have to identify your own challenges and adopt best practices that provide patients with the pricing transparency they want. Every lab is different – each with their own unique challenges as it relates to providing price transparency. Best practices to implement can include:
- Establish and support payer billing policies
- Perform benefit investigation
- Automate advanced eligibility
- Offer out-of-pocket estimate
- Preemptively address prior authorization and medical necessity requirements
At Quadax, we can help! Request a strategy call to discuss best practices to support your strategy and goals AND help you secure expected reimbursement of your tests and services.
Let's take on the revenue cycle together!
References:
- https://en.wikipedia.org/wiki/Consumerism: Aug 2019
- Shute, Debra A: Patient Access Antidote: Retaining More Revenue with Front-End Solutions; Dark Daily (2019), 4.
- Healthcare Consumerism & Your Revenue Cycle: Flip the Narrative and Build Loyalty Through Patient-Centric Tools and Processes; Quadax (2019), 2.
- http://www.norc.org/NewsEventsPublications/PressReleases/Pages/new-survey-reveals-57-percent-of-americans-have-been-surprised-by-a-medical-bill.aspx
- https://www.consolidatedcredit.org/infographics/medical-debt/#gref


